Join MIPS and Improve Patient Care
Unlock Rewards and Enhance Quality with QPP
2023 MIPS Performance
No Data Found
Merit-based Incentive Payment System (MIPS)
MIPS is one way you can participate in the Quality Payment Program (QPP). QPP is a federal program which reimburses Medicare providers, who are MIPS eligible clinicians for Medicare Part B covered professional services and rewards them for improving the quality of patient care and outcomes.
To participate in MIPS, you must select one of the available reporting options to fulfill the MIPS reporting requirements for each of the 4 performance categories:
Quality
This performance category assesses the quality of the care you deliver, based on performance measures created by CMS, as well as professional medical groups and interested parties. Quality performance category requirements differ based on the reporting option you select.
Promoting Interoperability
This performance category promotes patient engagement and the electronic exchange of health information using certified electronic health record technology (CEHRT) The Promoting Interoperability performance category requirements are the same for all reporting options.
Improvement Activities
This performance category assesses how you improve your care processes, enhance patient engagement in care, and increase access to care. Improvement activity performance category requirements differ based on the reporting option you select.
Cost
This performance category assesses the cost of the care you provide. We calculate cost measures, based on your Medicare claims, to determine the cost of the care you provide to certain patients. Cost performance category requirements differ based on the reporting option you select.
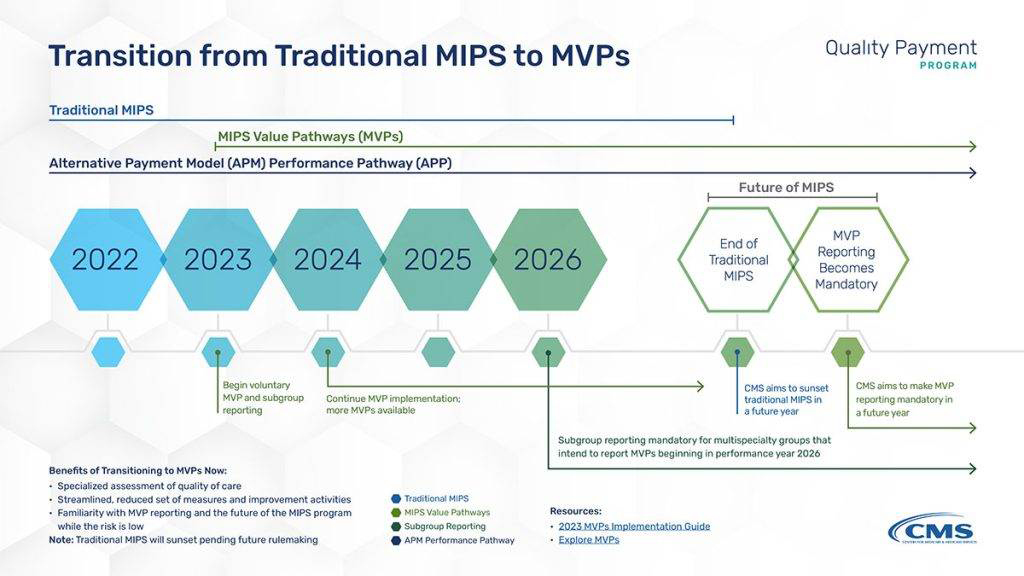
Transition from Traditional MIPS to MVPs
Starting in 2023, clinicians will have 3 MIPS reporting options: MVPs, traditional MIPS, and the APM Performance Pathway (APP). Starting in 2026, any multispecialty groups intending to report MVPs will be required to report as subgroups. CMS plans to sunset traditional MIPS in the future, at which point MVPs will become mandatory unless the clinician is eligible to report the APP.
What is the MVP Reporting Option?
MVPs are the newest MIPS reporting option (an alternative to “traditional MIPS” and “APM Performance Pathway (APP)”) that you can use to meet your MIPS reporting requirements.
Each MVP includes a subset of measures and activities that are related to a given specialty or medical condition. You can visit the Explore MVPs webpage to learn about the finalized MVPs available for reporting beginning in the 2023 performance year.
